Types of Skin Cancer
Skin cancers, like other cancer in the body, involve the uncontrolled proliferation of cells of the skin, leading to local symptoms of growth, bleeding, ulceration and in some cases, to local and distant spread of cells (metastases). A non-exhaustive list of contributing factors to skin cancer includes: fair complexion, red hair, total and intermittent exposure to ultraviolet radiation, ionizing radiation, psoralen exposure and immunosuppression.
When people talk about skin cancer, they are often referring to basal cell carcinoma (BCC), squamous cell carcinoma (SCC) and melanoma, however, there are also a group of rarer conditions whose associated manifestations include skin cancer, examples including mycosis fungoides, gorlin syndrome and torre- Muir syndrome, to name but a few.
Here we will only discuss the commoner types.
Basal cell carcinoma (BCC)
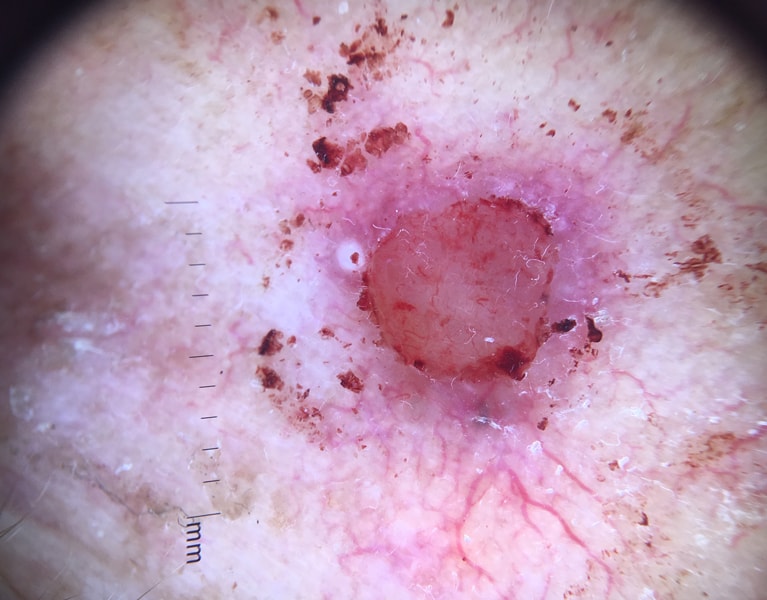
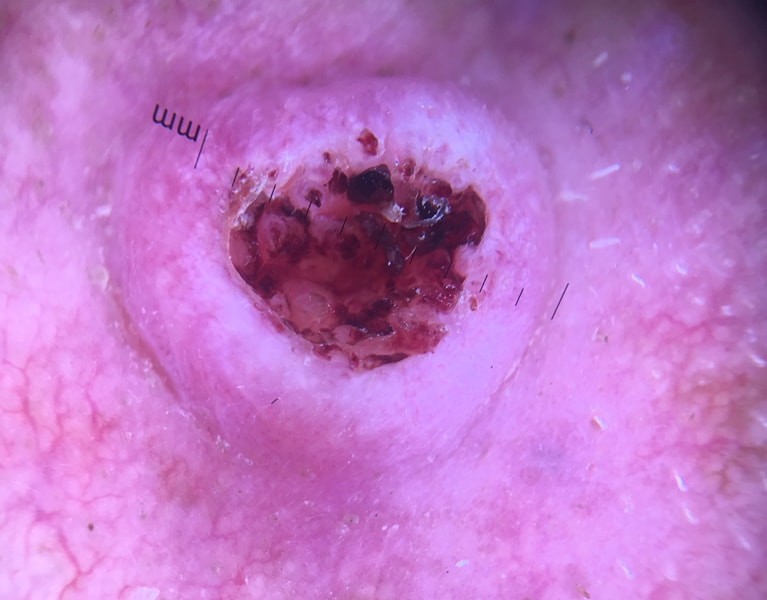
The commonest skin cancer, BCCs are a slow growing, locally invasive cutaneous tumors with spontaneous bleeding and ulceration causing pain. The molecular basis for this skin cancer is thought to arise from the inappropriate activation of the sonic hedgehog (SHH) and p53 pathways, leading to reduced tumor suppression and uncontrolled growth of basaloid epithelial cells. Complications can include local extension, recurrence and metastases (rarely). There are a number of histological subtypes including:
- Superficial: Diagnosed through biopsy and may be amenable to topical therapies and serial currette procedures as well as excision.
- Nodular: The commonest subtype. Again, diagnosed through biopsy and commonly excised surgically to achieve definitive treatment.
- Pigmented variants may mimic other skin condition, including melanoma. Microscopically, these tumors contain melanocytes and melanophages.
- Morphoeic, infundibulocytic and sclerosing subtypes. Somewhat more aggressive than the other subtypes, with more subclinical extension, though amenable to surgical removal.
- Basosquamous: A histological mix of the two most common skin cancers. Infiltrative and more aggressive in nature.
Squamous cell carcinoma
Derived from nests of squamous epithelial cells, this skin cancer type is also thought to arise through the inappropriate activation of the p53 cellular pathway via the aforementioned contributing factors. These carcinomas are thought to be more aggressive than BCCs, with a 5% 5 year metastases rate. Precursor lesion include actinic keratosis (also known as solar keratosis), erythroplasia of Queyrat and Bowen’s disease, described below.
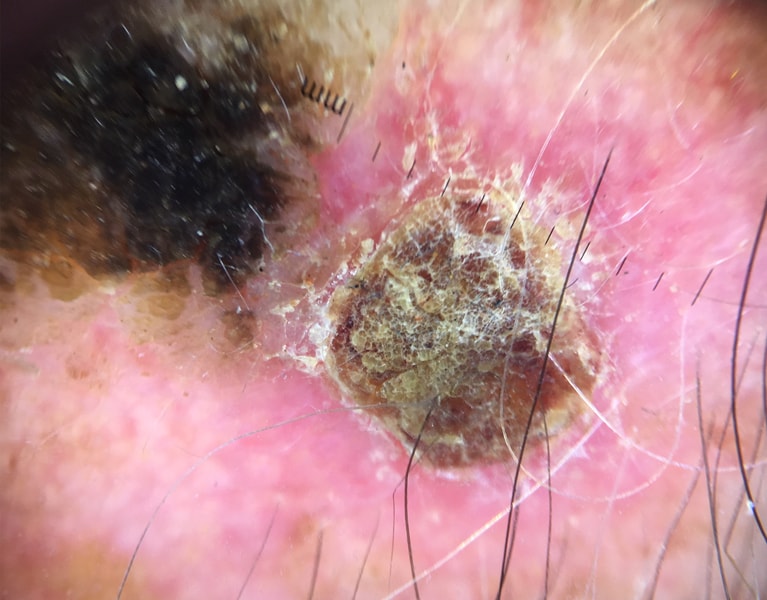
Actinic keratosis. Also known as solar keratosis and actinic cheilitis when it occurs on the oral mucosa, these lesions are thought of as a cancer precursors and are characterised as transient scaly red patches of skin, with abnormal keratinocytes found in the epidermis skin layer on microscopy. There are atrophic hypertrophic and acantholytic variants. These lesions are diagnosed through dermoscopy and readily amenable to cryotherapy, electrotherapy, topical creams and photodynamic therapy with a photosensitising agent.
Superficial squamous cell carcinoma (SCC). Also known as Bowen’s disease, this entity is diagnosed by biopsy, which demonstrates abnormal squamous cells throughout the entirety of the epithelial skin layer. Bowen’s disease is amenable to topical treatment or serial curette excision, as well as traditional surgical excision.
Keratoacanthomas are thought by some to represent a variant of well differentiated SCC. They are rapidly growing nodular lesion, often filled with a central core of keratin. In addition to the usual contributing factors, there are a few rarer syndromes as well as medications which may contribute to their development.
Invasive SCC. This skin cancer type has abnormal epithelial cells that have broken through the epithelium and into the dermis. It has many histological variants including basaloid, infiltrative, inflammatory, verrucous, follicular and spindle cell SCCs with markedly different prognoses based on these subtypes. Overall, SCC is a decidedly more aggressive cutaneous cancer than BCCs.
Melanoma
Malignant melanoma (MM) arises from the uncontrolled division and proliferation of the pigment producing melanocyte cells. Though most commonly arising from areas on the skin (cutaneous), a very small portion (2-7 cases per million persons) of primary melanomas arise from non-cutaneous locations, such as the eye, the nasopharynx, oral mucosa, genitourinary tract and gastrointestinal tract. The remainder of this discussion will focus only on cutaneous MM.
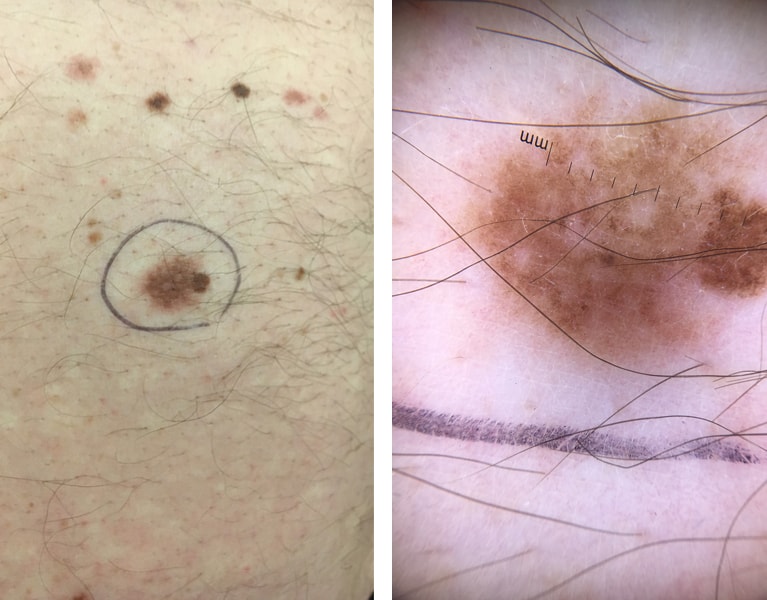
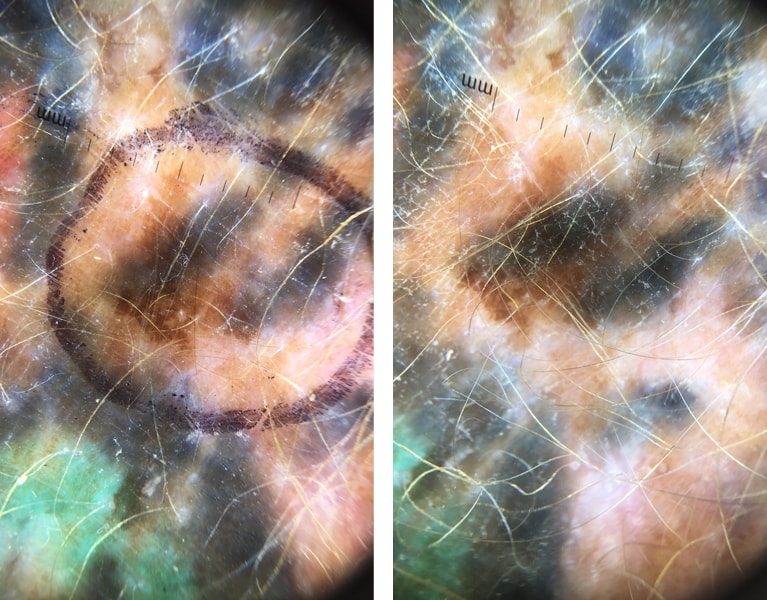
There are a number of factors that increase the likelihood of a melanoma, and again, this list is not exhaustive as large multivariate analyses of data continue to delineate contributing factors. However, we know that recently changing moles (particularly those with dermoscopic documentation of change), childhood UV exposure, episodic UV exposure, acquired melanocytic nevi, dysplastic nevi, prior melanoma and non-melanoma skin cancers, phenotypic variance (fair skin red hair blue eyes) and family history are all contributing factors.
A number of genetic mutations have been associated with the development of MM and these include mutations in the BRAF, NRAS, KIT, PTEN genes, which are mostly tumor suppressor genes.
The most important take home message is: If there has been any change, or if you are unsure, seek a medical opinion.
Clinically, there are four types: Superficial spreading melanoma Nodular melanoma Lentigo maligna melanoma and acral lentiginous melanoma (hands feet nails). Prognosis is dependant on a number of factors, including: diameter of the lesion, total area of the lesion, depth of the lesion and ulceration. There are also a number of histopathological factors, including mitosis rates, lymphovascular invasion and regression as well as its location on the body (TANS regions worser prognosis) and the presence of metastases.
Diagnosis of MM can only be made with an excisional biopsy, removing the entire lesion for histological analysis in its entirety. If confirmed, Wide Local Excision (WLE) must be undertaken within 4 weeks, the width of which is determined by the pathological results of the biopsy. In most cases, where the cancer has been picked up early, definitive cures can be achieved following WLE. In more advanced cases, chemotherapy, immunotherapy, radiation therapy and additional surgery may be required.